Virtual GLP-1 startups: Pill mills or the future of obesity care?
Acknowledgements: Thank you to my research collaborators, Dr. Namrata Hulawale, Allen Peng, Dr. Krishanga Srivastava, and Dr. Tarun Srivastava, who worked tirelessly on this project over the last three months!
Disclaimer: I’m an investor in Omada Health
GLP-1 medications like Ozempic, Wegovy, and Zepbound are reshaping modern medicine. Initially developed for diabetes, they are now widely used for obesity treatment and are under investigation for a wide range of other conditions, from kidney and heart disease to addiction to dementia. Some experts have called GLP-1s the most important drug class breakthrough in medical history, comparing their impact to the discovery of insulin.
The timing of their rise is notable. These drugs have come to market in a period of widespread adoption of virtual care. Digital health platforms were already set up to prescribe online, ship medications directly to patients, drive patient engagement, and operate outside of traditional insurance systems. That infrastructure made it easy for hundreds of companies to launch or pivot toward GLP-1 prescribing to meet demand quickly.
According to a 2024 KFF poll, 12% of U.S. adults say they’ve taken a GLP-1 medication. While most (79%) got their prescription from a primary care doctor or specialist, 11% used an online provider. That translates to roughly 3.4 million Americans who have received a GLP-1 prescription from a virtual platform.
Yet most primary care physicians (PCPs) are skeptical of telehealth platforms prescribing GLP-1s for weight loss. A 2025 survey of over 2,000 U.S. PCPs conducted by Omada Health found that two-thirds (67%) think these services may put their patients’ health at risk, and just 18% said they were comfortable with patients using them. Over half (57%) said they actively caution patients against getting GLP-1s from virtual providers, with their main concerns being overprescribing and lack of continuity of care.
At the same time, the median primary care visit is just 15.7 minutes, and most clinics do not offer weight care support, like nutritional counseling or support groups, to increase the chances of long-term success. Not to mention that there are fewer than 100 doctors who have completed a fellowship in obesity medicine and are actively practicing in the U.S.
In that context, it’s not surprising that patients are turning elsewhere. The status quo has not served them. Virtual platforms are often faster, easier, more affordable, and less judgmental than traditional care. For many, they represent the best path to accessing treatment.
I don’t think the question is whether weight care, and GLP-1s specifically, should be available virtually. It’s whether they’re being prescribed safely, supported appropriately, and offered by companies that put long-term patient health above short-term growth.
The surge in demand for GLP-1 medications attracted a wide range of virtual care companies. Some were built specifically for this moment, while others adapted existing models to capitalize on the opportunity. Broadly, they fall into three categories:
GLP-1-focused startups like Found and SkinnyRx that exist solely to prescribe weight loss medication.
Legacy weight and metabolic care platforms like Noom, Omada Health, and WeightWatchers that expanded into GLP-1 prescribing.
Broader virtual care platforms like Ro and Hims that include weight loss as part of a larger offering (most commonly longevity, hormone-replacement therapy, and hair loss).
These companies are scaling at an extraordinary pace. Remedy Meds, founded just 18 months ago, is already projecting $450 million in revenue this year and claims to be profitable. Hims & Hers generated $420 million from its GLP-1 business in the first six months of the year alone.
But no one has fully defined what responsible virtual prescribing of GLP-1s should look like. So I partnered with a team of researchers from Johns Hopkins Bloomberg School of Public Health to develop a set of principles for high-quality virtual weight loss care—a benchmark against which we measured the 39 companies listed above.
Of the 39 companies we reviewed, 13% are publicly traded and 44% are venture-backed. The venture-backed group has raised a combined $2.8 billion in funding, reflecting the intense investor appetite in the category.
Together, these companies account for the majority of GLP-1 prescriptions being written virtually today, and represent the full spectrum of approaches—from clinically rigorous, wrap-around care models to high-volume pill-pushing platforms.
⚖️ The 8 principles of responsible virtual GLP-1 care, and how these companies stack up
1. Expanding access and affordability of treatment
One of the strongest arguments for virtual prescribing is the increased access to life-changing medications.
Digital health companies are helping more people access safe, effective treatment for obesity and metabolic health, especially those who might otherwise be left out of traditional care. By removing friction points like long wait times, high costs, and stigma, virtual platforms make it easier for patients to get started.
Beyond simply being available quickly, many platforms have gone out of their way to increase access. Some, like Form Health, Calibrate, 9amHealth, Sesame Care, Teladoc, and Omada, partner directly with employers to offer GLP-1 programs as a covered benefit. Others work with benefits platforms for distribution, like Noom, which partnered with Collective Health, and WeightWatchers, which partnered with Personify Health.
While just six clearly advertise that they accept health insurance, several offer concierge tools to help patients navigate insurance. We were impressed by Ro’s insurance coverage tracker, which gives users a personalized report detailing their insurance coverage for GLP-1 medications and estimated copay and/or out-of-pocket costs.
2. Following clinical guidelines with reasonable eligibility checks
We observed significant variability in the thoroughness of clinical evaluations and the clarity of treatment eligibility criteria.
While most platforms take care seriously, many others seem to have low clinical standards. We observed significant variability in the thoroughness of clinical evaluations. Some platforms allow free-text entry for both medications and medical conditions, which may increase the risk of users overlooking relevant health issues. Some platforms even allow patients to proceed to payment without confirming standard clinical eligibility.
Last summer, a WIRED investigation found it “shockingly easy” to access GLP-1s. The reporter lied about having a high BMI, and ReflexMD, Alan Meds, Henry Meds, Ro, and Get Thin MD still gave her an Rx (Hims & Hers was the only one to not). None of the platforms required a synchronous video call with a clinician, except Henry Meds, which did lead to a medication adjustment.
Our secret shopper audit tested multiple profiles, including users with normal BMI and past disordered eating. In one case, we were recommended GLP-1s even though the user was underweight (5’7” and 110 pounds). This suggests that a few companies are approving prescriptions for people who do not meet clinical criteria.
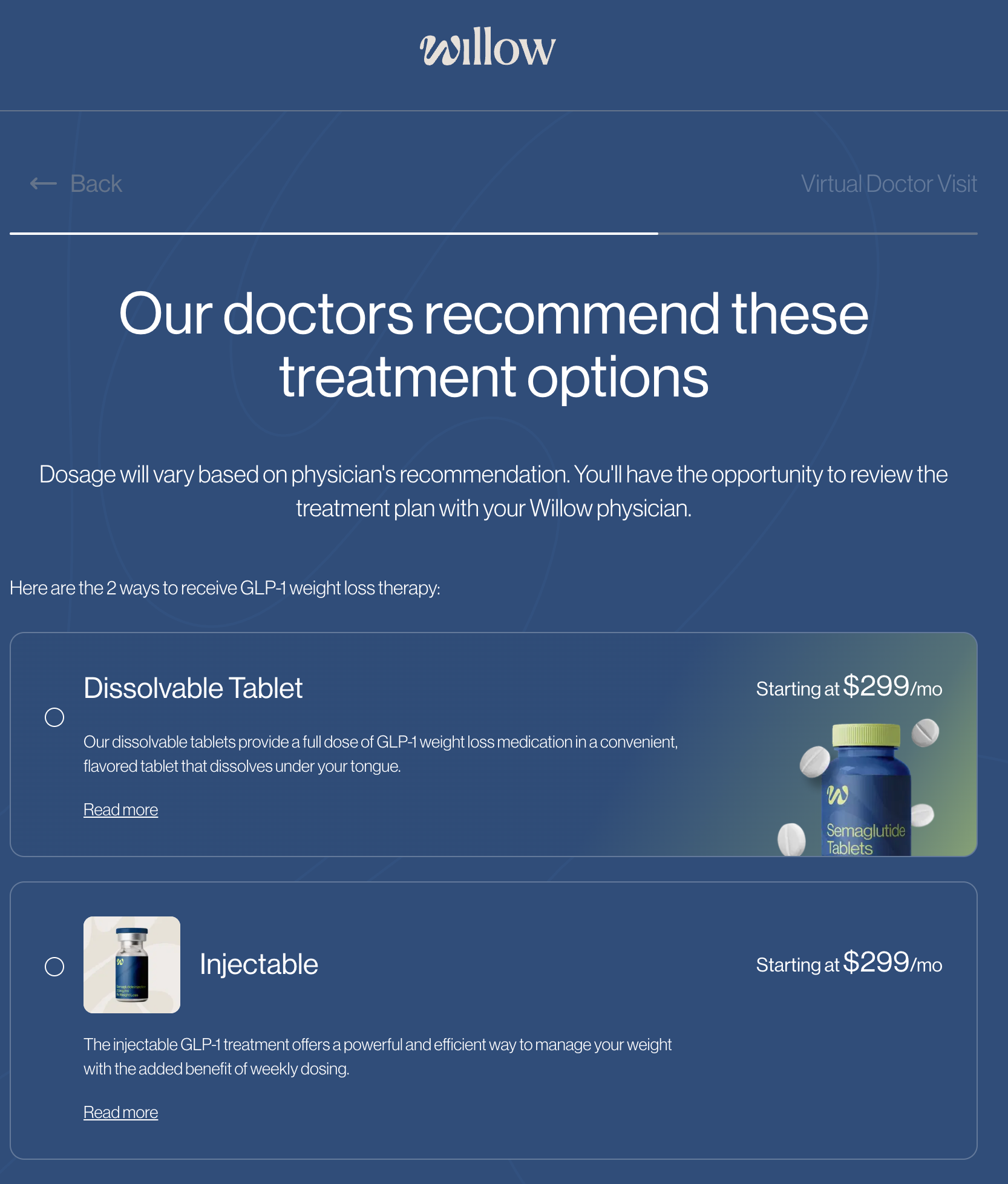
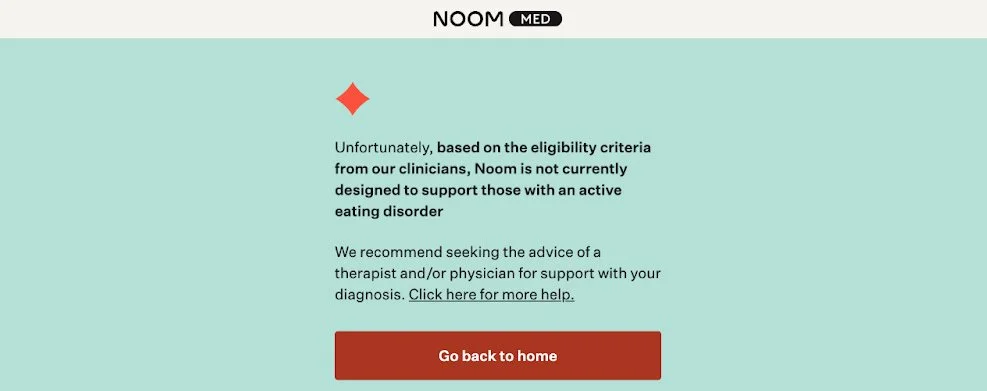
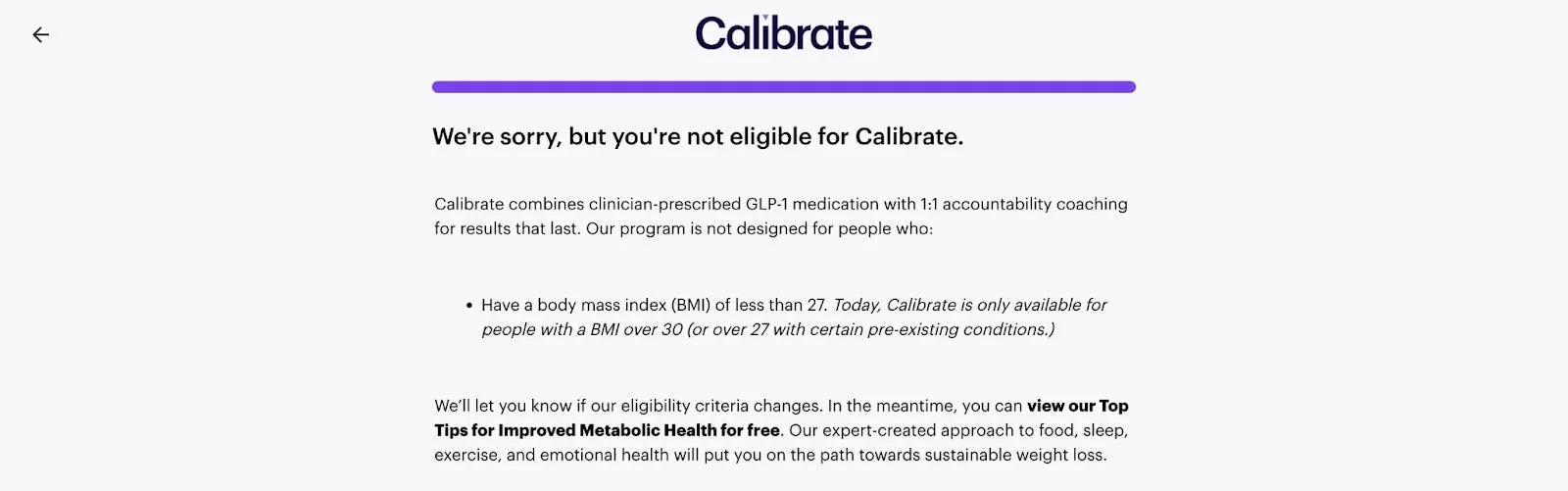
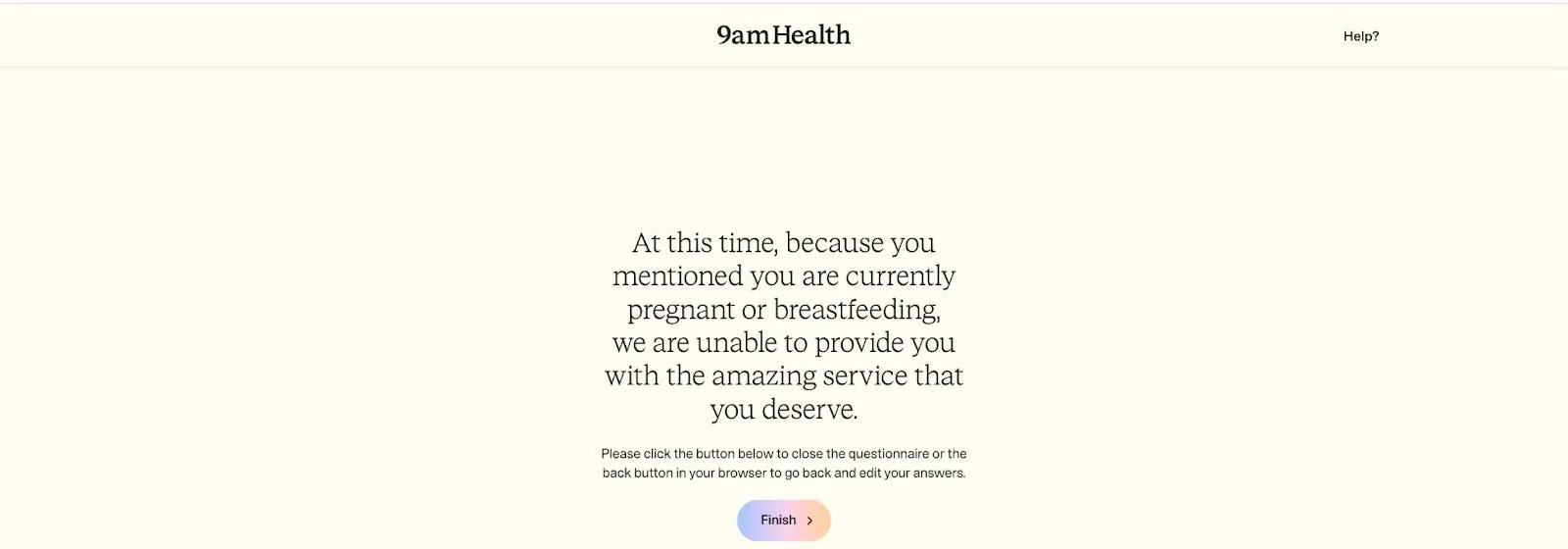
However, we did find that the majority of platforms rejected users who did not qualify based on FDA treatment eligibility criteria:
3. Providing wrap-around support for nutrition, behavior change, and mental health
GLP-1 medications are approved for chronic weight management only as an adjunct to diet and exercise—not as quick fixes that “cure” obesity after a few doses. In fact, obesity treatment guidelines emphasize that GLP-1 medication should be combined with a high-protein diet, increased physical activity, and behavioral interventions (self-tracking, therapy, group support, dietary education, etc.). When patients receive this support along with medication, they are more likely to stay adherent and make the lifestyle changes necessary for long-term success.
In practice, however, many patients are prescribed the drug with little additional support, and a significant number stop treatment early. The result can be worse than where they started: the return of prediabetes, hypertension, dyslipidemia, and weight regain, sometimes compounded by muscle loss that leaves them in poorer overall health.
This problem isn’t unique to virtual providers—GLP-1 “pill mills” exist in person, too. The difference is that digital health can scale poor prescribing practices far more quickly, amplifying both their reach and potential harm.
On the flip side, digital health has the potential to scale low-cost, effective treatments by combining GLP-1 prescribing with tools that promote adherence and drive meaningful behavior change.
Across the 39 companies we reviewed, 87% offered structured wrap-around support, including one or more of the following:
Tracking and goal-setting tools
Meal plans and recipes
Nutrition counseling
Behavioral health tools
Virtual support groups or community chat
Virtual workouts and exercise plans
Lab monitoring
4. Offering ongoing monitoring, labs, and long-term treatment planning
The prescription is just the beginning. Safe and effective GLP-1 treatment requires ongoing monitoring and a plan for long-term management. This includes baseline labs, follow-up testing, vital sign monitoring, and dose adjustments based on the patient’s individual response.
Many platforms, including Hone Health, incorporate lab work and monitoring of key vitals into their programs. This data helps clinicians adjust dosages, detect potential side effects, and ensure the patient’s overall health is improving.
Noom goes one step further with its SmartDose program, a highly personalized, "low and slow" titration method that effectively doubles the number of dose steps and includes more frequent check-ins than the standard protocol. By tailoring each dose adjustment to the patient's specific progress and side effects, the guiding principle is to find the lowest effective dose that comfortably sustains long-term results, rather than rushing to the maximum dose in the shortest time possible.
5. Ensuring clear safety disclosures, especially around compounded drugs
Compounded drugs are custom medications prepared by a pharmacist for an individual patient, often when an FDA-approved product is not medically appropriate, or when the approved drug is in short supply and meets the conditions set out in federal law. In the case of GLP-1s, this can mean semaglutide or tirzepatide made in a compounding pharmacy rather than dispensed as an FDA-approved brand-name product.
66% of the platforms we reviewed offered compounded GLP-1s. We don’t think compounded drugs are inherently bad. In fact, their presence has helped providers meet demand and lower the cost (the price discrepancy between compounded and brand-name might even be partially responsible for encouraging pharmacos to drop their prices).
However, compounded drugs are not FDA-approved and may be associated with higher safety concerns and product quality issues. Companies that sell compounded medications should disclose that these drugs are not FDA-approved and haven't undergone the same rigorous testing for safety and effectiveness as FDA-approved drugs.
6. Marketing services ethically and without stigma
Patients are often first exposed to these medications through ads on Meta platforms (Facebook, Instagram) or TikTok, where many of the companies we reviewed were actively advertising.
Responsible marketing avoids body-shaming imagery, exaggerated claims, or urgency-driven gimmicks. Yet too often, ads minimized risks or promoted unrealistic outcomes. Willow, for example, ran ads encouraging patients to cancel their gym membership and promised rapid weight loss—messaging that directly contradicts clinical guidelines and feeds into unhealthy narratives (they also prescribe to patients regardless of BMI). As I wrote about here, their ads trivialize the use of GLP-1s and cross a line into irresponsible promotion.
By contrast, companies like LifeMD, AgelessRx, and Midi Health framed ads around licensed providers, FDA-approved options, and ongoing care. These examples demonstrate that it’s possible to build demand without misleading patients or trivializing the risks associated with treatment.
7. Prescribers who have expertise in obesity medicine
While any licensed physician can prescribe GLP-1s, the nuances of safe and effective treatment are best handled by specialists in obesity medicine, primary care, endocrinology, or related fields.
In our review of provider listings, many platforms were staffed primarily by emergency or internal medicine clinicians, with relatively few showing American Board of Obesity Medicine (ABOM) certification. This does not mean the clinicians are unqualified—but it does mean that many online patients are not receiving care from those with formal expertise in obesity care.
8. Transparency about leadership and clinical teams
Finally, we believe that patients deserve to know who is behind the platforms providing their care. Yet we found surprising gaps in transparency.
Some of these companies had no listed leadership and no presence on LinkedIn. In some cases, we couldn't identify a single executive or clinician publicly associated with the platform.
In other cases, a clinician’s involvement seemed to be overstated. For example, neither the doctor nor the pharmacist listed on Levity's About Us page had the company listed on their personal LinkedIn pages.
Lack of transparency around the team isn’t breaking any laws, but it feels… sketchy. And in a space where patient trust is already fragile, opacity about who is actually running and overseeing care can deepen concerns about accountability and credibility.
By contrast, platforms like Form Health and Omada Health prominently feature their clinical leadership, credentialed providers, and advisory boards. This visibility builds confidence that prescribing decisions are made responsibly and that the people working for the company stand behind its care.
⭐ Platforms that follow these principles earn higher patient ratings
When platforms follow these principles, the payoff is better care and better outcomes. Responsible virtual GLP-1 care leads to:
Higher patient satisfaction and trust
Better adherence and persistence with treatment
Improved and more sustainable weight loss
Stronger metabolic health outcomes
Fewer preventable side effects and complications
Reduced risk of weight cycling and rebound
It also shows up in patient experience. When you look at customer reviews (we used Trustpilot as a proxy, where most platforms had thousands of ratings), the companies that adhered most closely to these principles earned meaningfully higher scores.
Across the 39 platforms we reviewed, the average Trustpilot rating was ~4.0/5.0 stars, but the range was dramatic. At the low end, 54% of Willow reviews are low-star (1 and 2 star) with an average rating of 2.9, and OrderlyMeds had 30% low-star reviews and an average rating of 3.7.
By contrast, Hone Health (4.9 stars, ~2% low) and SkinnyRx (4.6 stars, 5% low) were standouts in terms of customer satisfaction.
Where this is headed
GLP-1s aren’t going away. Neither is virtual care. The real question is whether this space will mature into a legitimate, responsible arm of obesity medicine or be dismissed as a chaotic market of pill mills.
Startups have the chance to lead in delivering comprehensive, evidence-based weight care at scale. The best programs combine medication with wrap-around services: clinical oversight, behavioral coaching, nutrition support, and long-term planning. These services are essential to making treatment safe, effective, and sustainable.
Digital health companies are uniquely positioned to deliver this kind of care—flexible, accessible, and affordable. But that promise comes with responsibility. Companies that cut corners, skip clinical standards, or mislead patients damage trust in the entire industry.
To realize the full potential of GLP-1s, we need digital health. And we also need accountability. This moment is a test—not just of these medications, but of whether our industry can rise to meet the challenge of long-term, whole-person health. And I’m optimistic.